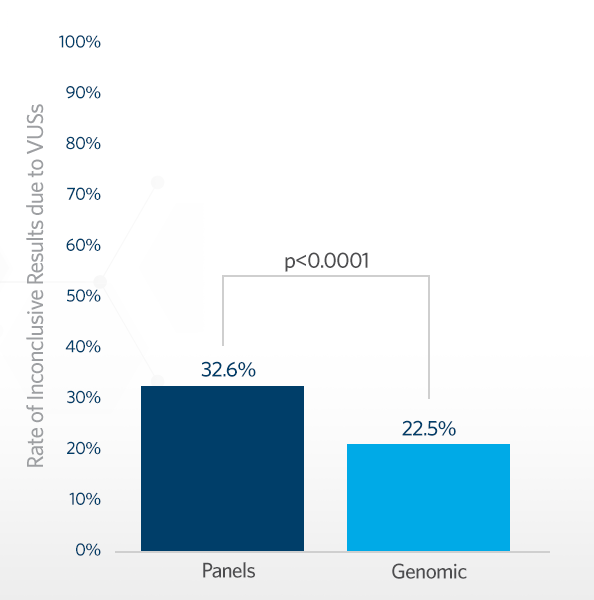
Are uncertain results (variants of uncertain significance, or VUS) more likely in multi-gene panels (MGP) or whole exome- and genome-based (WES/WGS) tests? Ambry recently participated in a study led by the Medical Genomic Initiative (MGI) comparing the VUS rates for MGP and WES/WGS. The study, conducted across 19 clinical laboratories in North America, collated results for more than 1.5 million patients with a variety of clinical presentations tested on a wide range of platforms. The data revealed that, despite capturing and analyzing far more genes and variants compared to MGP, WES/WGS testing demonstrated a 10% lower rate of reported VUS (22.5% vs. 32.6%).
The Challenge of VUS
Healthcare providers must often choose between these testing approaches. MGPs contain genes selected based on the clinical features and come in a range of sizes from a few genes to several thousand. In contrast, WES/WGS examines all genes and reports out variants with clinical significance to a proband. Both testing approaches can yield variants of uncertain significance (VUS), which are genetic alterations whose clinical significance is not yet fully understood, complicating their interpretation and management. VUS leave patients and healthcare providers without a definitive answer or clear path forward for medical decision-making and often leads to further testing, added stress, and potential downstream costs.
How Reporting Practices Impact VUS Rates
Some providers have selected a MGP approach based on an assumption that VUS rates would be lower. However, evidence now demonstrates this isn’t the case. It may seem counterintuitive but stems from the reporting practice distinctions between the different testing approaches:
- In MGP testing, typically all VUS identified in the targeted genes are reported.
- In WES/WGS, reporting considers clinical overlap and additional family data to determine which VUS are reported, therefore reducing the overall number of reported VUS.
Trio testing, where family members are sent for analysis alongside a patient’s sample, also helps reduce VUS rates in WES/WGS. Having family members’ data can help clarify the significance of an alteration seen in a patient. For example, if an alteration is seen in a healthy parent, it lowers the chance that it may be causing a childhood-onset condition. This study found that in a trio setting, both WES and WGS saw significantly lower rates of VUS compared to samples sent with only one or no relatives.
Panel Size Matters
Small panels, with less than 10 genes, had a VUS rate of 6%, but this rate steadily increased with panel size and more than ¾ of patients tested on panels with 200 genes or more had an inconclusive rate due to a VUS. This highlights the importance of considering gene content when designing panels. While it may seem logical that the larger the panel, the more likely it is to identify a diagnostic finding in a patient, this is accompanied by an increased VUS burden.
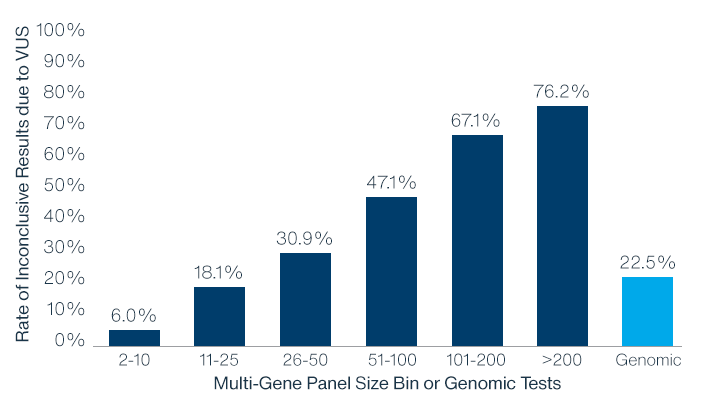
Panel Content Also Matters
It is crucial that laboratories carefully evaluate the gene-disease relationship, the evidence that a gene causes a disorder, and that the disorder is appropriate for the clinical purpose of the panel, before including it on an MGP. If there is insufficient evidence that a gene causes a disease, then by default all variants within that gene cannot be more than a VUS. The addition of genes with limited evidence for causing a disorder will not increase diagnostic yield for MPGT but has the potential to increase VUS identification.
Panel Testing Still Has a Place as a Diagnostic Tool
This is not to say MGPs are not a powerful diagnostic tool! Especially for conditions like inherited cancer risks where the causative genes are well known and current clinical guidelines have encouraged good MGP reimbursement by payers, MPGT remains an effective and practical option for healthcare providers.
This study underscores the vital partnership between healthcare providers and laboratories in optimizing the application of genetic testing and critically reviewing testing practices. The clinical impact of these findings is substantial, not only for healthcare providers but also for third-party payers as they evaluate the clinical utility of WES/WGS and their offered coverage options. Ultimately, this research emphasizes the importance of staying current with evolving genetic testing practices to provide the best care for patients on their diagnostic journeys.
Learn More
To see a complete review of the study data and hear discussion from the lead author, view this EducateNext webinar featuring Dr. Heidi Rehm.
For even more, check out this free downloadable PDF, Research For Your Practice: Exome- and Genome-Based Testing Have Lower VUS Rates than Multi-Gene Panel Testing.



