National Minority Health Month (NMHM) dates back to April 1915 when Booker T. Washington established the National Health Improvement Week (later known as National Negro Health Week).1,2 The goal then, as it remains today, was to improve the health and wellbeing of underserved or minority populations. This can only be done by building awareness of inequities that minorities face when accessing healthcare, identifying the barriers that exist, and systematically working to reduce and eliminate those barriers.3 However, despite this being NMHM’s 109th birthday, inequities still exist, especially in the genetic counseling field.
Although genetic counseling is now more widely available and the cost of genetic testing has significantly decreased over time, minority patients do not have the same access to these services as others. Multiple studies have found that providers are more likely to refer White patients for a family history of cancer compared to other races/ethnicities (Black, Asian, and Hispanic).4-6 And when patients of other races/ethnicities are referred, it’s more likely because of a personal history of cancer, and in many cases, the cancer is already at an advanced stage.4-6 There are many explanations for this, including limited time in appointments, limited knowledge about cancer genetics, limited family history collection during the appointment, and implicit bias against minority patients. As we work to address and overcome these limitations, we can start to provide more proactive care for our minority patients and improve health outcomes when it comes to reducing the risk of cancer and detecting it sooner.
Figure 1: Black Patient Outcomes from Digital Patient Management Program
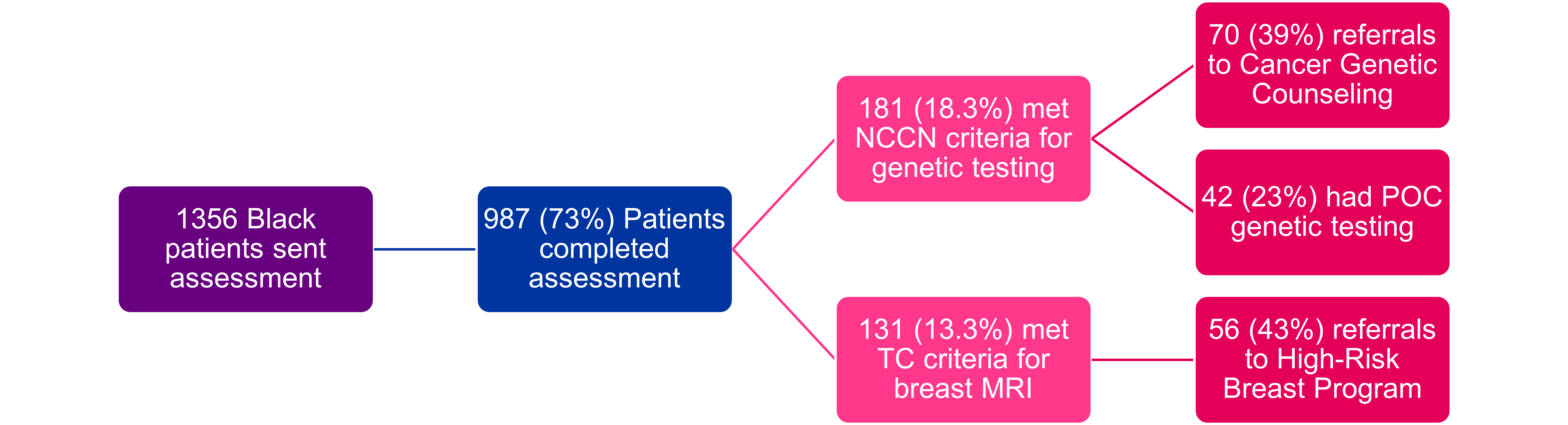
We have started this work at TriHealth by working with our gynecology offices to roll out the Ambry CARE Program® (CARE), which includes digital cancer risk assessment tools. Prior to an annual gynecology visit, patients receive an assessment by text/email that asks about their medical history, reproductive history, and personal/family history of cancer. All patients are asked the same set of questions, and all patients’ responses are analyzed the same way to determine if they meet cancer genetic testing and/or breast MRI criteria. The cancer risk assessment process is standardized, meaning it’s the same from patient to patient, provider to provider, and practice to practice. Standardizing the cancer risk assessment process helps to eliminate implicit bias at multiple levels of the healthcare system. With this change, providers also have information about a patient’s genetic and breast cancer risk prior to the appointment, saving time in the appointment and allowing for a focused conversation about available genetic services and how this information can be used in their health management plan.
Figure 2: Provider Referral Rates of Black Patients Before and After Digital Patient Management Program
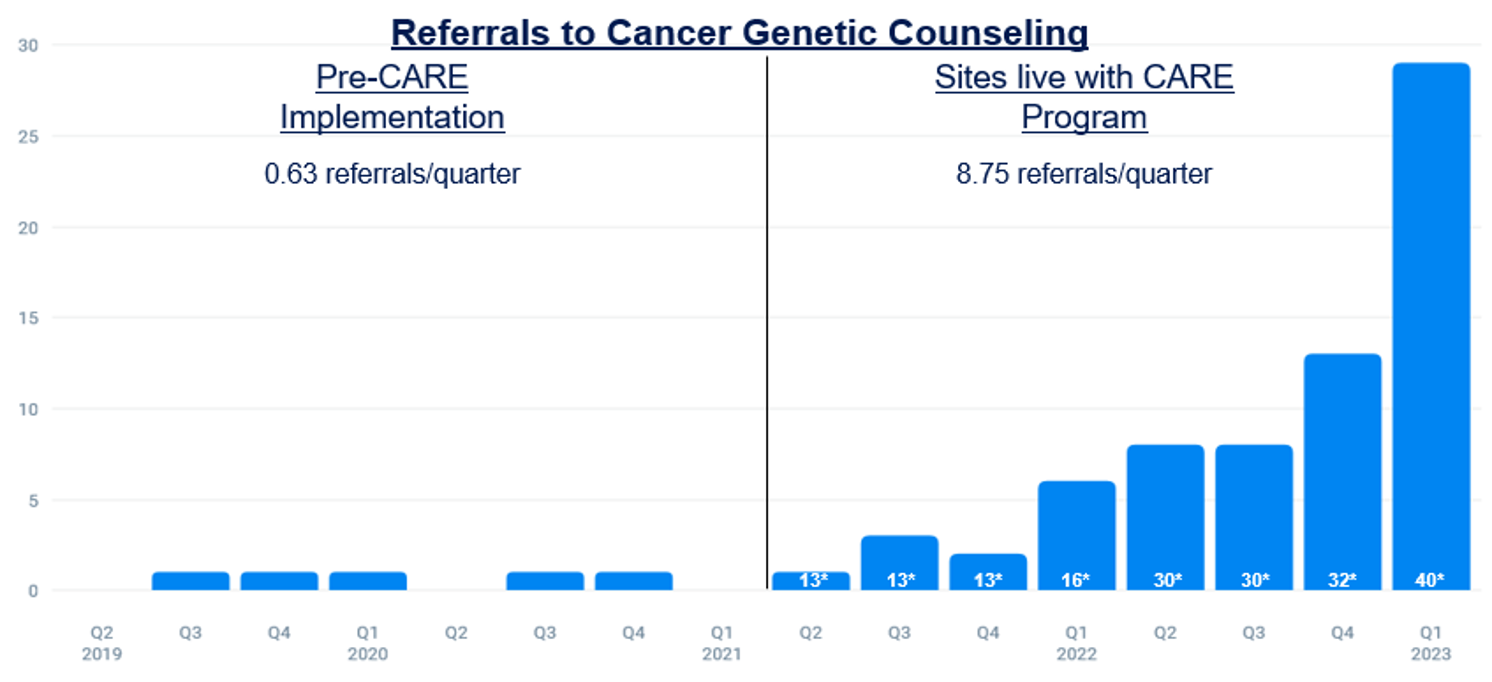 1300% Increase in Referrals to Cancer Genetic Counseling
1300% Increase in Referrals to Cancer Genetic Counseling
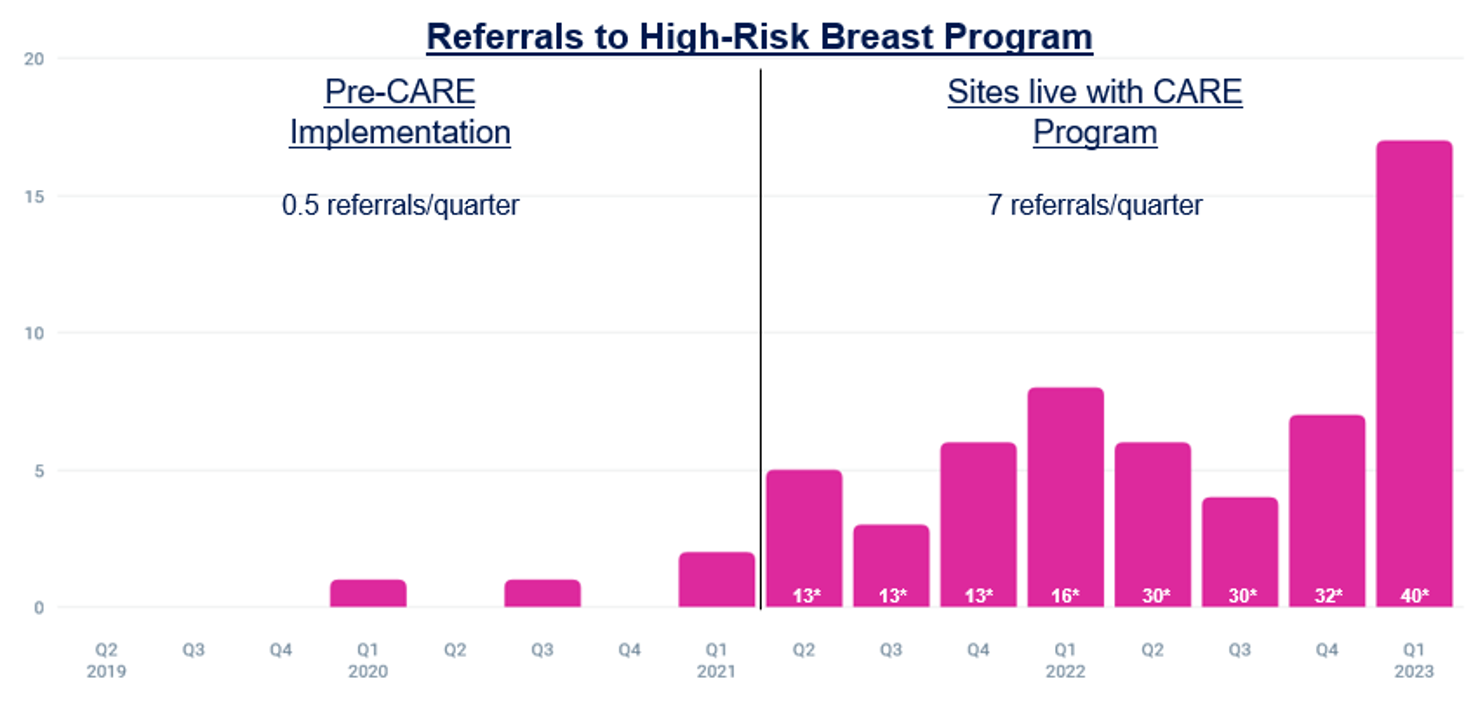
1300% Increase in Referrals to High-Risk Breast Program
*Number of CARE providers is shown in white in each column
Since rolling out this program in 2021, we have seen a significant increase in referrals to cancer genetic counseling and the high-risk breast program for our Black patients. Prior to the CARE Program, we received 6 referrals of Black patients to cancer genetic counseling over the course of 30 months (40 providers total). After the CARE Program was rolled out, we received 70 referrals of Black patients over the course of 28 months from the same group of providers. Of these patients, 24 completed their appointments. We’ve also had a significant increase in referrals to the high-risk breast program with 4 referrals of Black patients in the 30 months prior to the CARE rollout, and 56 referrals of Black patients in the 28 months after the program went live. We are not aware of any other major practice changes during this time and believe that the increase in referrals is due to the use of digital cancer risk assessment tools across all gynecology offices.
Figure 3: Referral Outcomes
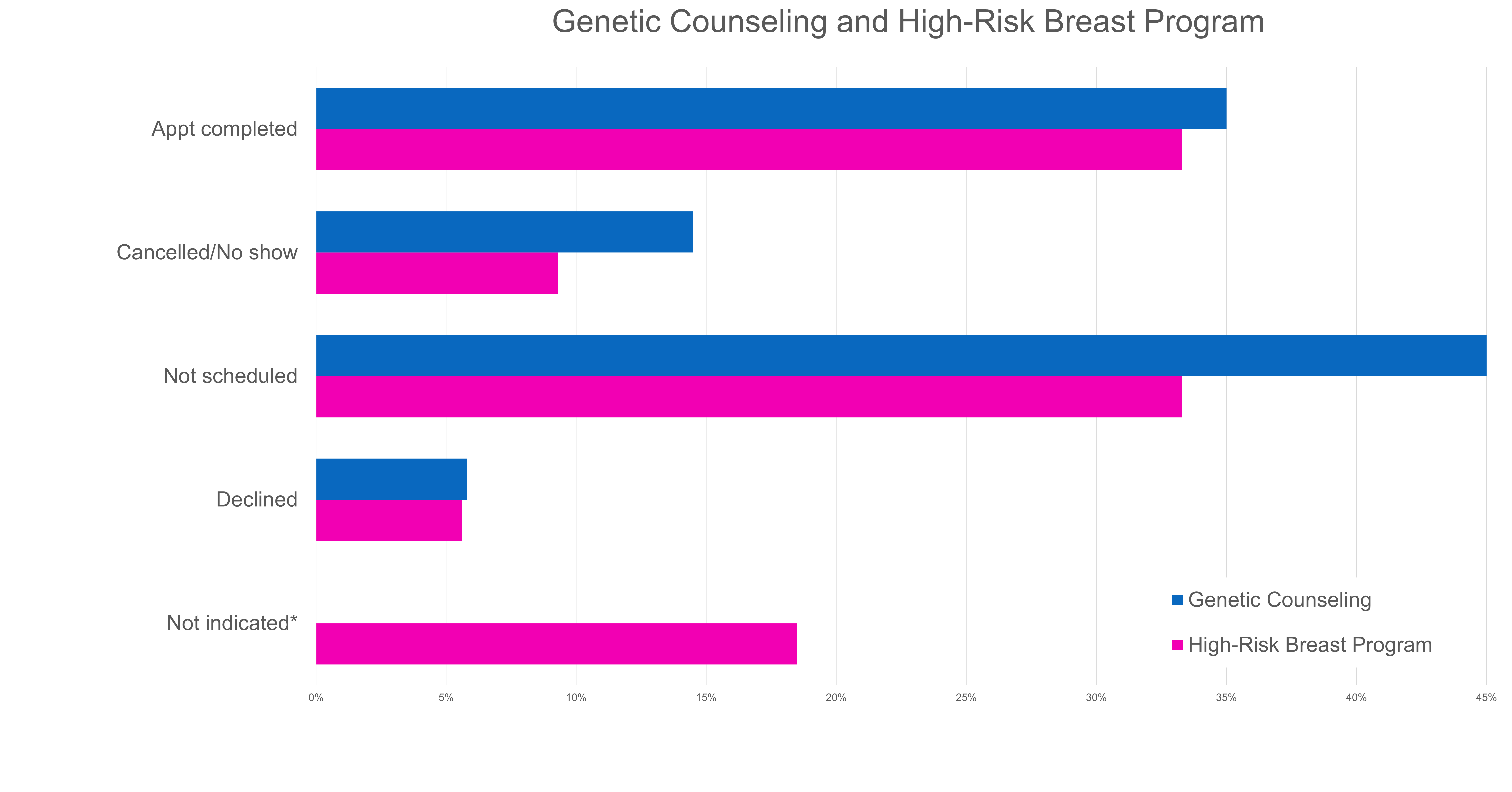
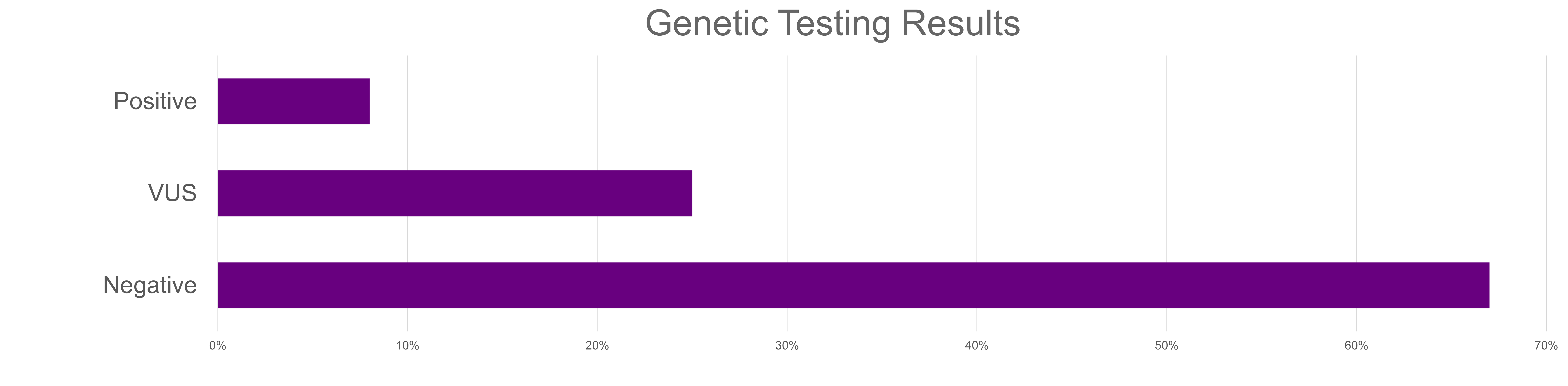
The CARE Program has helped providers better identify minority patients that meet criteria for genetic testing and breast MRI and facilitate conversations about these services. The standardized questions have also helped reduce implicit bias since all patients receive the same questions, and all results are analyzed in the same way. However, while these numbers show that the CARE Program is increasing awareness of and access to genetics services for our Black patients, our work doesn’t stop here. As more patients complete the questionnaire, we will be analyzing outcomes for other minority groups. We are also investigating other barriers to care that may exist, such as the time and cost constraints of an appointment after a referral is placed. We want to ensure patients are not just being identified, but are also able to reliably access genetic services. The work may have started in 1915, but we must continue to address existing disparities in order to ensure everyone has equitable access to quality healthcare.
Sources
1. “National Negro Health Week”: 1915 to 1951 – Rediscovering Black History (archives.gov)
2. https://www.nps.gov/bowa/booker-t-washington-created-national-negro-health-week.htm
3. National Minority Health Month (nih.gov)
4. Chapman-Davis E, Zhou ZN, Fields JC, Frey MK, Jordan B, Sapra KJ, Chatterjee-Paer S, Carlson AD, Holcomb KM. Racial and Ethnic Disparities in Genetic Testing at a Hereditary Breast and Ovarian Cancer Center. J Gen Intern Med. 2021 Jan;36(1):35-42. doi: 10.1007/s11606-020-06064-x. Epub 2020 Jul 27. PMID: 32720237; PMCID: PMC7859010.
5. Williams CD, Bullard AJ, O'Leary M, Thomas R, Redding TS 4th, Goldstein K. Racial/Ethnic Disparities in BRCA Counseling and Testing: A Narrative Review. J Racial Ethn Health Disparities. 2019 Jun;6(3):570-583. doi: 10.1007/s40615-018-00556-7. Epub 2019 Apr 8. PMID: 30963508.
6. Armstrong K, Micco E, Carney A, Stopfer J, Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA. 2005 Apr 13;293(14):1729-36. doi: 10.1001/jama.293.14.1729. PMID: 15827311.



