A conversation with Arlene Jacobs, MD, Plano Women’s Healthcare
Caitlin Reid, CGC: Dr. Jacobs, you’ve been passionate about screening your patients for hereditary cancer. Can you tell us why you use hereditary cancer risk assessment in your OB/GYN practice?
Arlene Jacobs, MD: Many of my patients see me not only as their OB/GYN, but as their primary care provider. I form deep connections with my patients, and they trust me to care for them as a “whole” person.
Since about 1 in 4 OB/GYN patients meet guidelines for hereditary cancer testing,1 I want to be instrumental in identifying them—and helping them receive the important, timely care they need.
OB/GYNs are at unique points in a patient’s overall healthcare journey. We can help identify patients who may be at risk for inherited cancer—like breast and ovarian—during their annual well-visits and inform them of their options for further care. Additionally, ACOG2 and other associations have published guidelines that help us to know when hereditary cancer testing is appropriate for our patients.
What’s more, patients may not be aware of their family history of cancer or the implications it has for their own health. I help my patients understand their risk by conducting thorough family health history assessments before each well-visit and recommend genetic testing when appropriate. These assessments can easily be done by paper or digital form—or even be fully automated via an end-to-end risk assessment program, which I personally use to save even more time.
This testing plays a crucial role in identifying patients at risk for certain types of cancer, allowing for early intervention and personalized care plans.
Caitlin Reid, CGC: You mentioned hereditary breast and ovarian cancers specifically. Can you talk more about the type of hereditary cancer test you find most useful as an OB/GYN?
Arlene Jacobs, MD: Breast and ovarian are the main inherited cancers that come to mind for an OB/GYN office, but as I mentioned, we care for the “whole person”—seeing them for their preventive/well-woman visits. While genes like BRCA1 and BRCA2 are most well-known for those cancers, there are many other genes related to those cancers (and other cancer types).
I prefer to use comprehensive, guideline-informed, multi-gene panels that test for the most common types of hereditary cancer—even beyond breast and ovarian—such as colorectal, pancreatic, etc. These are also cancers that are found in my patients.
Just as I would refer a patient to get a Breast MRI, or to a breast surgeon based on a positive BRCA2 result, I also just as easily refer them to a colorectal surgeon if there is a pathogenic mutation on MLH1, for example.
Furthermore, Genetic Counselors are an excellent, consultative partner in helping to discuss genetic testing options, interpret results, and to provide guidance to providers and patients alike. So, if I ever receive a result that requires additional consultation, I reach out to my genetic counseling partners for further care guidance.
Caitlin Reid, CGC: That’s a great point about the value of comprehensive hereditary cancer testing and how you conduct specialist referrals.
Can you share an example of a patient case you had where they had a positive result?
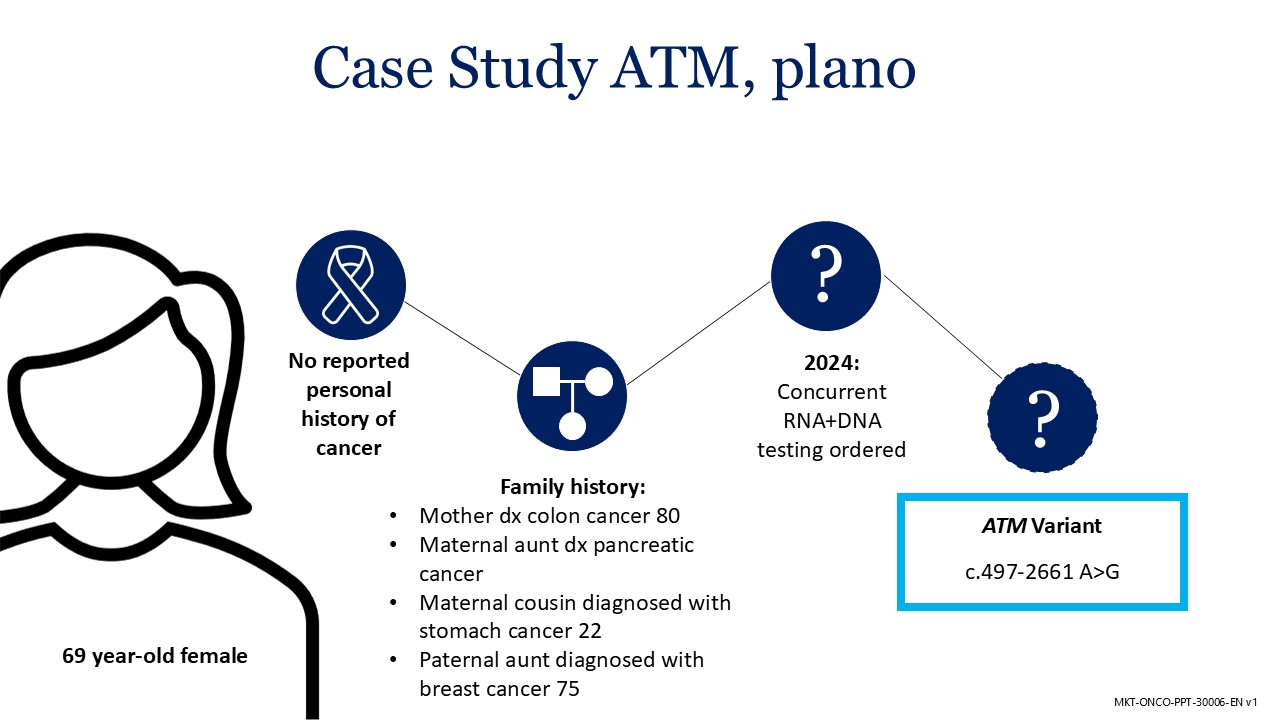
Arlene Jacobs, MD: Certainly. One of my patients, a 69-year-old female, had no reported personal history of cancer. When I reviewed her hereditary cancer risk assessment results, her family history of cancer indicated that she should get hereditary cancer testing to assess her own personal risk. She has a mother who was diagnosed with colon cancer, an aunt diagnosed with pancreatic cancer, a different aunt was diagnosed with breast cancer, and a cousin diagnosed with stomach cancer.
I ordered a comprehensive, multi-gene panel with RNA, and the results came back indicating she has an ATM variant. This variant increases her risk for breast and other cancers. I referred her to a breast surgeon, and she is doing well now. This testing also led for her two daughters and one son to get the same testing—and one of her daughters (mid-30s) was also found to have the same ATM variant. So, this testing not only helped my patient get early, critical care—but her daughter as well.
Caitlin Reid, CGC: That’s wonderful that she and her daughter were able to get identified early and receive the life-saving care they needed.
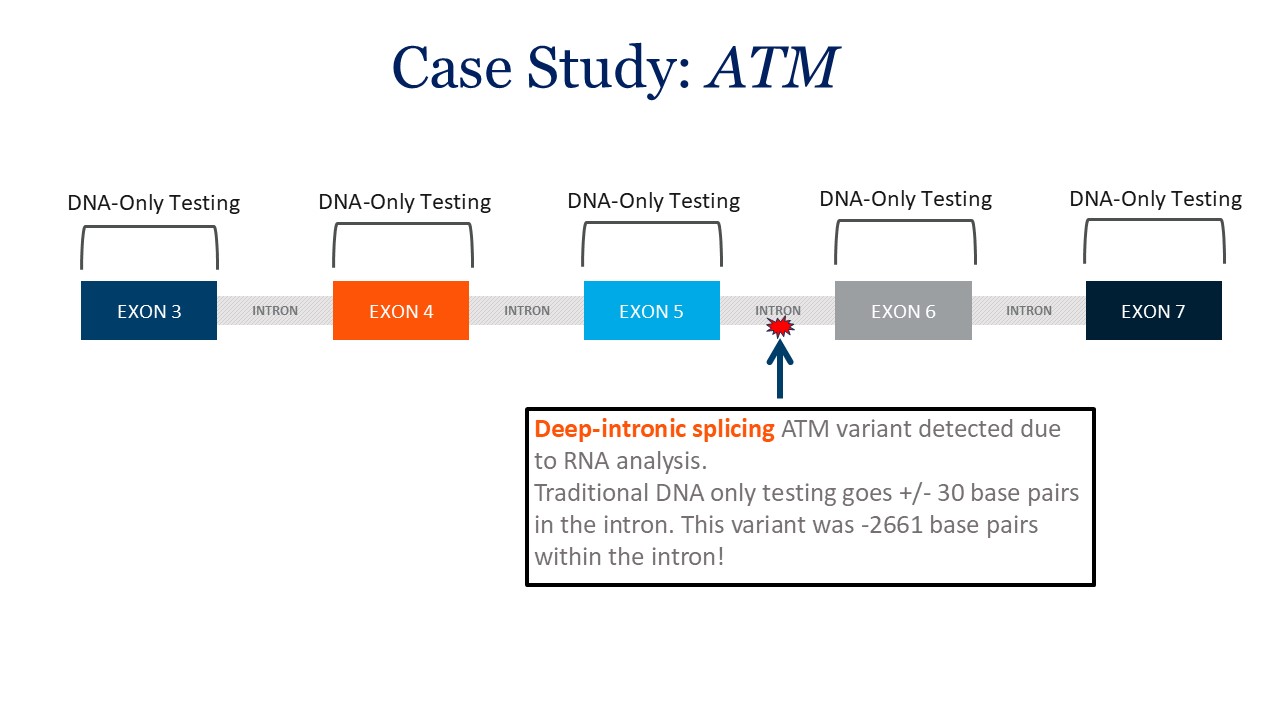
The other interesting point about that patient example is that your ordered concurrent RNA alongside the DNA testing. By running the RNA concurrently with the DNA, the ATM mutation was able to be found in the deep intron. If RNA were not ordered (or if it were a reflex test), the mutation would not have been found.
Arlene Jacobs, MD: Excellent point, Caitlin. I include the concurrent RNA as part of the panel order because it finds patients like this one, that other testing may miss. Plus, it doesn’t affect turnaround time and is little to no cost to my patients.
Caitlin Reid, CGC: Thanks for sharing your insights, Dr. Jacobs. Are there any final thoughts that you’d like to share?
Arlene Jacobs, MD: OB/GYNs provide comprehensive care that addresses all aspects of a woman's health. My recommendation is: “Don’t miss the 1 in 4”—you can help save their life. Screening, risk assessment, and testing for hereditary cancer are integral parts of this holistic approach, ensuring that patients receive the best possible care throughout their lives.
___
Sources
1. Bucheit et al. Opportunity for Cancer Prevention: 1 in 4 Unaffected Women Meet Hereditary Cancer Testing Criteria [26O]. Obstetrics & Gynecology 133():p 169, May 2019.
2. ACOG COMMITTEE OPINION, Number 793. Obstet Gynecol. 2019