Welcome to the Gene Scene! Each week, we will explore a gene from the ACMG Secondary Findings list—genes identified by the American College of Medical Genetics and Genomics as having clear, actionable health implications. These genes are included because they’re linked to serious but preventable or manageable conditions when identified early. Here, we focus on the condition that led to the gene’s inclusion on the list, providing clear, relevant information that supports your clinic. To subscribe to the Gene Scene, contact your local GSL or send a request to info@ambrygen.com.
To access the Gene Scene archives, visit our blog.
Clinical Phenotype Summary:
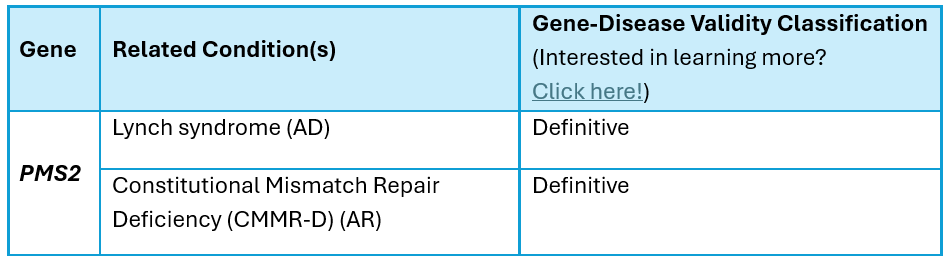
The PMS2 gene (NM_000535.5) is located on chromosome 7p22.1, encodes the mismatch repair endonuclease PMS2 protein, and contains 15 coding exons. Pathogenic variants in this gene are known to cause Lynch syndrome (also known as hereditary non-polyposis colorectal cancer or HNPCC), which is inherited in an autosomal dominant fashion, and constitutional mismatch repair deficiency (CMMR-D) syndrome, which is inherited in an autosomal recessive fashion.
PMS2-related Lynch syndrome is characterized by an increased risk for the following cancers:
• Colon cancer (8.7-20% cumulative lifetime risk)
• Endometrial cancer (13-26% cumulative lifetime risk in females). Specifically, the cancer risk is demonstrated to be increased for individuals over the age of 50
• Risks for cancers of the:
• Ovary
• Small bowel
• Stomach
• Pancreas
• Biliary tract
• Renal/bladder (urothelial)
• Sebaceous glands (a variant of Lynch syndrome also known as Muir Torre syndrome)
• Central nervous system may be elevated in individuals with a PMS2 pathogenic variant compared to the general population
• Some studies have estimated that mutations in mismatch repair (MMR) genes may be related to an approximately 2-fold increase in prostate cancer risk; however, new data suggests that this risk may be attributed primarily to mutations in MSH2, and that this risk may be less significant for other MMR genes
• Overall, lifetime colorectal and endometrial cancer risks for individuals with PMS2 pathogenic variants are estimated to be lower than those associated with pathogenic variants in the MLH1 and MSH2 genes
• In addition, variable expressivity is observed; therefore, cancer risks will differ based on individual and family history.
Loss of function has been reported as the mechanism of disease for PMS2-related Lynch syndrome CMMR-D is characterized by café au lait macules and an increased risk for hematologic malignancies, brain tumors, and early-onset Lynch syndrome-associated cancers. Individuals of reproductive age are at 25% risk of having a child with CMMR-D with each pregnancy when both biological parents have a pathogenic variant in PMS2. Biallelic loss of function has been reported as the mechanism of disease for CMMR-D.
Unique Considerations:
• When inherited in an AD manner, PMS2 causes Lynch syndrome. When inherited in an AR manner, biallelic PMS2 mutations cause CMMR-D.
• PMS2 has a known pseudogene, PMS2CL, which can complicate testing for exons 11-15.
Clinical Resources:
Ambry Knows Genes:
Scientific Posters:
Peer-Reviewed Publications:
• Somatic Tumor Profile Analysis in a Patient with Germline PMS2 Mutation and Synchronous Ovarian and Uterine Carcinomas (July 2021)
Citations:
• Dominguez-Valentin M et al. Genet Med, 2020 01;22:15-25 PMID: 31337882
• Ten Broeke S et al. J Clin Oncol. 2018 Oct 10;36(29):2961-2968 PMID: 30161022
• Møller P et al. Gut, 2018 07;67:1306-1316 PMID: 28754778
• Wang C et al. JNCI Cancer Spectr. 2020 Apr 23;4(5):pkaa027 PMID: 32923933
• Ryan S et al. Cancer Epidemiol. Biomarkers Prev. 2014 Mar;23(3):437-49 PMID: 24425144
• Aronson M et al. J Med Genet. 2022 Apr;59(4):318-327 PMID: 33622763
• Ambry Genetics Gene-Disease Validity Scheme
Each week, we explore a gene from the ACMG Secondary Findings list—genes identified by the American College of Medical Genetics and Genomics as having clear, actionable health implications. These genes are included because they’re linked to serious but preventable or manageable conditions when identified early.
To learn more about the ACMG Secondary Findings list, click here.